Driving Better CDI Performance with Standardized Education
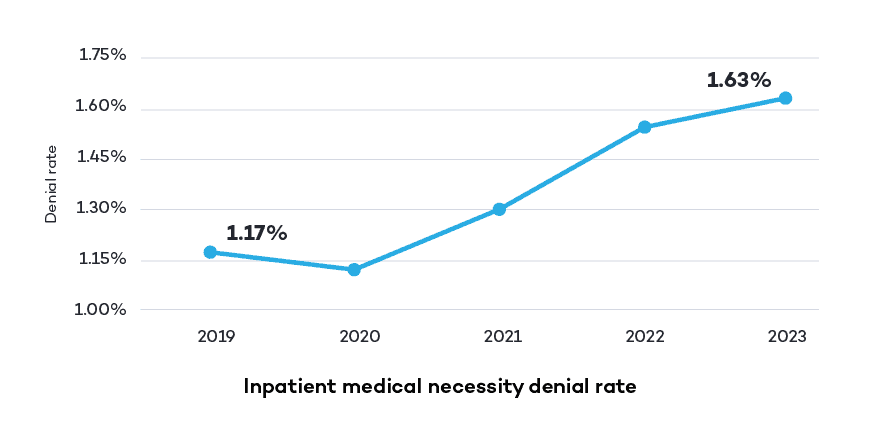
Healthcare providers can easily find themselves in a reimbursement bind as commercial payers and Medicare Administrative Contractors (MACs) increasingly scrutinize more than just coding accuracy when reviewing claims, and that can have a negative impact on CDI performance. More and more, payers are challenging the medical necessity of procedures, especially those with a high-cost treatment, resulting in more denied claims and delayed payments. In fact, our 2023 Revenue Intelligence Data Insights Report found that from 2019 to 2023, there has been a nearly 40% increase in medical necessity denial rate for inpatient claims.
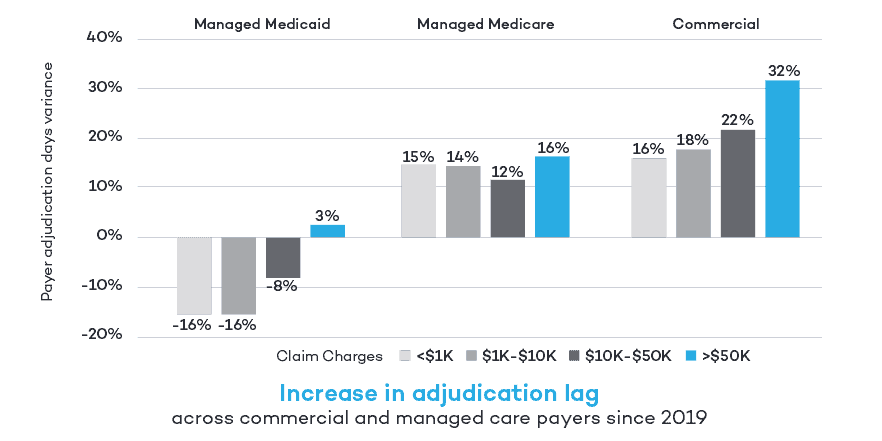
For high dollar claims greater than $50,000, commercial payers saw more than a 30% increase in days to adjudicate claims compared to 2019.
Coder shortages disrupting the RCM process
Hospitals and health systems are not the only organizations impacted by the ongoing shortage of qualified, experienced medical coders. Commercial payers and MACs are also short staffed and often compete for any available coding talent. The shortage is exacerbated by the complexity of disparate payer rules, documentation requirements for supporting level of care decisions for shorter hospital stays, and the increase in home-based high acuity care. One of the best strategies for overcoming these new challenges is investing in CDI specialist education and training for existing staff.
Education drives CDI performance improvement
Our education use case involves a CDI team with a director and 12 CDI specialists of varied backgrounds—ADNs, BSNs, foreign medical graduates, and a chiropractor. One team member held credentials for CCS (certified coding specialist), CCDS (certified clinical documentation specialist), and CCDS-O (certified clinical documentation specialist-outpatient), another one for CCS and CDIP (certified documentation integrity practitioner), and a third for CCS, CDIP, and CCDS.
There is a clear struggle in the medical profession to find a standardized way to assess CDI specialist skills and knowledge gaps. Anecdotal evidence from discussions with other teams reveals that CDI training is often of the ‘telephone’ or ‘train-the-trainer’ variety where one specialist trains the next one who then trains the next one and so on. Eventually enough noise gets introduced into the training to degrade its quality and original intent. When that’s compounded by annual coding guideline changes and quarterly coding clinics, the risk of coding errors in claims data grows exponentially. So, what does that mean for a program’s day-to-day or year-to-year effectiveness? That’s what we set out to determine.
Expert intervention delivers tangible results
We began by establishing baseline data on our team which looked at reviews, queries and impacts to revenue, CMI1 (Case Mix Index) and GLOS2 (Geometric mean Length of Stay), which we continue to monitor monthly. The team also participated in a baseline assessment of CDI and coding knowledge. We then had our CDI team participate in a five-day comprehensive education series that covered everything a CDI specialist should know, from coding guidelines to base rates and CMI to sequencing and coding opportunities broken down by MDC.
We reinforced this education with two-hour working sessions with each specialist twice a month for three months and performed monthly QA audits for a period of three months. We continued monthly education meetings where coding clinics, diagnoses and coding guidelines were discussed. After 12 weeks, the specialists took another knowledge assessment.
The proof is in the performance
The results from this seven-part education program not only showed improvement, but they also exceeded expectations. Each of the CDI specialist’s assessment scores improved at the 12-week mark, those that improved but did not pass were put into further remediation with continued working sessions and QA audits and retested after an additional 12 weeks. At the end of 24 weeks, all specialists had passed the assessment. Metrics improved in every area measured, and some were substantial, like a 300% plus increase in impact queries. But there was one improvement that sums up the program’s success—the 150% increase in net revenue capture.
To learn more about Clinical Documentation Integrity, visit R1RCM.com/cdi-solutions.
1 CMI: A hospital’s CMI represents the average diagnosis-related group (DRG) relative weight for that hospital. It is calculated by summing the DRG weights for all Medicare discharges and dividing by the number of discharges.
2 GLOS: The condition or diagnosis-specific length of stay reasonable for a substantial number of patients, assuming optimal recovery, decision-making, and health system design and performance.